I’ll never forget my first time.
It was when I was at university and sharing a house with other students. Our dinner routine was always the same: cook together, eat together, and sprawl on the sofa – or even fall straight into bed.
Lying on the sofa one evening, I felt a sudden, sharp pain in my chest, and a slight feeling of pressure. It wasn’t too painful and was over quickly, so I didn’t give it much thought.
Over the following weeks, however, I experienced the same discomfort again and again, at varying degrees of intensity. A visit to the doctor revealed that I was suffering from heartburn. Thinking about it afterward, the diagnosis totally added up: the symptoms were always worse when I lay down after eating, especially if I’d over-indulged.
The doctor prescribed me a proton-pump inhibitor, or PPI, which is an acid-reducing medication. The heartburn went away on that drug, and stayed away even when I discontinued the medication. At least for a while. When the reflux finally flared up again in the form of airway reflux, I had to figure out what was going on and how to fix the problem permanently. That’s when I started Refluxgate.
But let’s talk about you. Do you have heartburn? If yes, let me share with you the most important things I have learned about heartburn from my research and interviews over the years:
1. Acid Reflux
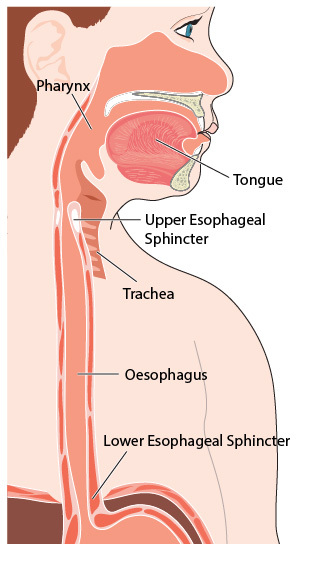
Heartburn occurs when gastric juices flow back from the stomach into the esophagus. Its medical name is gastroesophageal reflux disease (GERD), or simply “reflux.”
Acid reflux is especially likely to occur if you lie down with a full stomach.
The reason for this is simple. While you’re standing, gravity helps keep the contents of your stomach where they should be: in your stomach. When you lie down, however, it’s easier for gastric juices to flow back into your esophagus. Reclining, for example in a chair, or leaning back on your sofa, can have a similar effect, to a lesser degree.
This is not to say that you can’t get heartburn while standing. However, most people experience the worst symptoms when they eat and then lie down.
2. What Causes Chronic Heartburn?
Reflux is a protective function that prevents the stomach from overstretching. If you eat too much, the stomach releases pressure into the esophagus.
When this happens on a minor scale, it’s not a problem. However, some people are more prone to reflux than others - this can be due to an anatomical dysfunction.
There are different causes for reflux. One is a too weak “lower esophageal sphincter” (LES). This is the valve that sits between the stomach and the esophagus.[1]
In some people, this valve is simply not strong enough to perform its function effectively. It might have become damaged from decades of overeating.
Another cause can be a too tense pyloric sphincter (the valve at the exit of the stomach). In that case, the pressure in your stomach will be higher than usual, which means you will get reflux more easily.
Either way, what it comes down to is that you need to be careful to avoid reflux triggers, or to fix the cause of your reflux.
3. Inflammation of the Esophagus
The constant reflux of gastric juices causes the esophagus to become inflamed. That state of inflammation is called esophagitis.
If the reflux is untreated, a complication known as Barrett’s esophagus can develop over time. Barrett’s esophagus is characterized by a change in the esophageal mucosa and is considered to be a form of pre-cancer. It doesn’t happen overnight, but over a long period of time. This is why reflux should not be left untreated for too long.[2]
Heartburn remedies alone are not enough – they must be accompanied by a change in your diet.
Acid-reducing drugs do not prevent malignant changes in the esophagus. To prevent cancer, you have to tackle reflux at the source.
Another thing worth mentioning is that patients can have chronic heartburn without visible signs of inflammation in the esophagus. Our bodies react differently to acid exposure. While some people react with much inflammation but little pain, others might react with low inflammation but severe pain.[3],[4]
Sadly, not every physician knows this. That’s why some patients get negative test results and are told they have no reflux and it’s all in their head - despite that, their heartburn is very real.
4. Heartburn, Chest Pain, Spasms, and More
The main symptom of acid reflux is commonly described as heartburn, but that’s not an entirely accurate description.
Many acid reflux patients experience a burning pain. But not all do.
For me, it was more pressure and stinging than burning. Other patients get chest pain, or spasms.
Why is there this wide variety in symptoms?
I mentioned earlier that reflux often causes inflammation of the esophagus. When you look at many online articles and even medical literature, it sounds like heartburn is just caused by reflux and inflammation and that’s it.
This simplified explanation is why many patients with untypical symptoms fall through the cracks when it comes to diagnosis and treatment. In reality however, reflux is more complex.
5. Even Light Reflux Can Irritate Nerves
Heartburn is caused by nerves that have become sensitive to your chronic reflux. Each time you reflux, those nerves are stimulated, and you feel heartburn. Or, to be very specific, the acid sensitive TRPV1 receptor is what causes this type of pain.[5],[6]
This is also why people can experience heartburn without any inflammation in the esophagus. Even small amounts of reflux can increase the expression of this TRPV1 receptor, which then leads to increased pain.[7]
In simpler words, you can get heartburn even from light reflux, if your body is sensitive to it.
You can see how people can fall through the cracks during diagnosis, as physicians might not see signs of significant reflux, while the patient’s pain is very real.
6. Chest & Backpain, Spasms, Swallowing Problems
Next to heartburn, there are also indirect symptoms of reflux. Those symptoms are caused by reflux damaging the esophagus. As a result, this organ stops functioning the way it should.
How does it feel when the esophagus stops working properly?
One example is a feeling of squeezing and spasms in the chest. That feeling means that the esophageal muscles are contracting incorrectly.
Another indirect reflux symptom is chest pain. People might also describe it as back pain, as we do not always feel the pain at the point where it really originates.
Problems with swallowing are connected to reflux as well. When we swallow, we basically just shove food down our esophagus. However, food does not just fall into the stomach from there. Instead, the esophagus rhythmically contracts in a wave like manner to transport food down. Reflux damages that function and swallowing can become difficult.[8]
However, only some patients experience these indirect symptoms.
7. Other Digestive Symptoms
Frequent heartburn indicates that the digestive system has fallen out of balance. It makes sense that if you have reflux, you are more likely to experience other digestive symptoms sooner or later.
These are a few of the other symptoms that can (but do not necessarily) occur alongside heartburn:
- Stomach pain
- Bloating
- Nausea
- Constipation
- Diarrhea
- Frequent burping
- Regurgitation
- Sour or bitter taste in the mouth
8. Reflux Can Affect the Airways
We often see adverts for heartburn medications, especially on TV. As a result, everybody had heard of heartburn, even people who have never experienced it. But few know that reflux can also affect the respiratory tract.
Typical symptoms of airway reflux include:
- Hoarseness
- Coughing
- Frequent throat clearing
- Asthma
- Other breathing difficulties
- Sore throat
- Excessive mucus in the throat
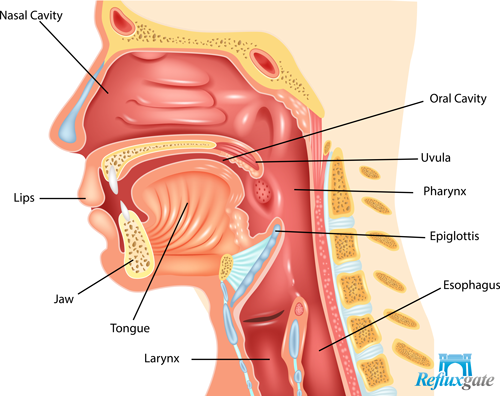
The symptoms of respiratory reflux are very similar to those of other diseases, including pollen allergies. This makes diagnosing it very tricky, even for doctors. Sadly, misdiagnosis of respiratory reflux is more the rule than the exception.
There are a few terms used for this airway type of reflux, e.g. laryngopharyngeal reflux (LPR) and silent reflux.
9. Diagnosis Is Usually Done Through Symptoms
Heartburn is such a clear-cut symptom that it’s often all that’s needed for a doctor to make a diagnosis.
In cases where additional diagnostic procedures are required, the patient must see a gastroenterologist. A gastroenterologist specializes in the digestive system. If your gastroenterologist decides to order additional tests, these will usually be:
- Gastroscopy
- 24-hour pH monitoring
- Manometry (measures the function of the esophagus & its valves)
Parallel to 24-hour pH monitoring, your doctor may also run an impedance test, which essentially records reflux by observing pressure changes in the esophagus. This offers a more accurate diagnosis than pH testing alone. However, not every specialist has the necessary equipment for impedance testing.
In simple cases, tests are rarely done. Reflux tests are time-consuming, expensive and unpleasant. What’s more, they are never 100% accurate, which can result in misdiagnosis.
Because of this, tests are generally only carried out if:
A. The symptoms are unusual.
B. The heartburn does not go away with treatment.
Additionally, it can take weeks or even months to get a specialist appointment. This is a long time to continue struggling with the pain. It also gives reflux more time to damage the esophagus.
Instead, it’s preferable to begin treatment straight away. If the symptoms disappear within a few weeks of treatment, this means that the diagnosis was correct and that no further tests are needed.
10. Heartburn Medications: The Fight Against Acid
In most cases, heartburn is triggered solely by stomach acid.
A variety of drugs target stomach acid. These drugs work either by neutralizing acid or by preventing it from being produced in the first place.
There are three main types of acid-combating drugs:
A. Antacids
Antacids are minerals that neutralize acids. You can find plenty of antacid brands in your local drug store, like Tums or Alka-Seltzer. You can even make your own at home, by using baking soda.

For people who suffer from heartburn only occasionally, antacids can be very useful.
In most cases, however, they are not an adequate solution.
B. Proton Pump Inhibitors (PPIs)
Proton Pump Inhibitors, or PPIs for short, drastically reduce the production of stomach acid.
In theory, they can prevent up to 98% of acid production. This is because PPIs destroy the stomach’s “proton pumps,” which play a vital role in acid release.
The problem is that the body replenishes these pumps continuously, which is why acid production increases again as the PPI dose wears off. This means that the average level of acid reduction decreases gradually as the day progresses. Depending on the dose, total daily acid production can be reduced by 60% to 80%. While the level may vary, this is still a massive change in the digestive process.
This significant reduction in acid production reduces the irritation of the esophagus. The result is less heartburn.
C. H2 Inhibitors
H2 inhibitors, also known as H2 receptor antagonists, reduce the stomach’s production of acid. Some well-known drugs are ranitidine (Zantac), cimetidine (Tagamet), famotidine (Pepcid), and nizatidine (Axid).
Nowadays, they tend to be used only rarely, since they’re less effective at reducing acid than PPIs.
For nocturnal reflux, however, H2 inhibitors can still provide significant relief. They work better on an empty stomach, while PPIs mostly reduce acid production after meals. Because of this, proton pump inhibitors are sometimes combined with an H2 inhibitor at bedtime.
One advantage of H2 inhibitors is that they have less detrimental impact on the natural digestive processes than PPI. Also, H2 inhibitors are not addictive, unlike PPI.
11. Proton Pump Inhibitors Are Overprescribed and Dangerous
PPIs are achieving record profits for pharmaceutical companies, who have marketed them aggressively as a miracle cure for heartburn.
As a result, proton-pump inhibitors have long been readily prescribed by doctors.[9]
In recent years, however, the long-term side effects of PPIs have become clearer.
Disruption of the Bacterial Balance
Nowadays, most people are aware that we have both good and bad bacteria living in our intestines.
The good bacteria live in a symbiotic relationship with our bodies. We help each other. Good bacteria create some of the nutrients our bodies need, support our immune system, and prevent bad bacteria from multiplying.
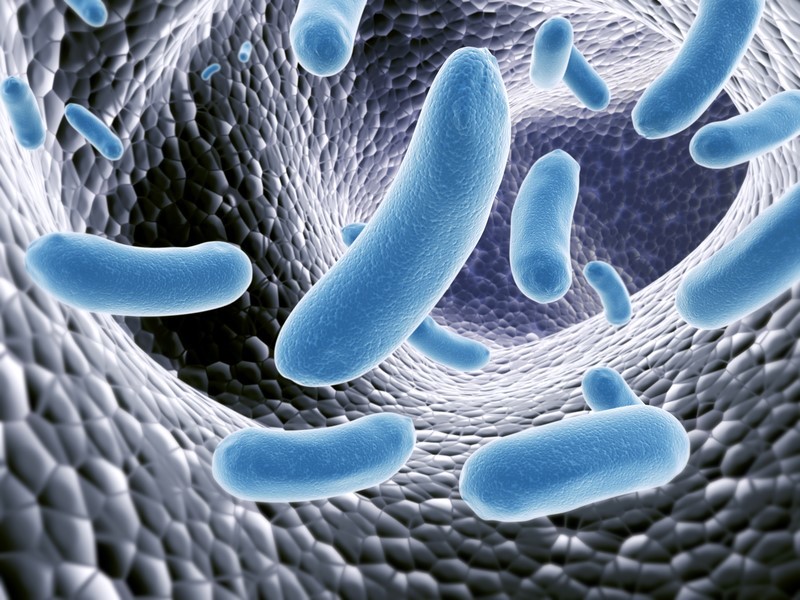
Unfortunately, the delicate balance between good and bad bacteria can easily be destabilized, for example by antibiotics.
Heartburn medication can damage this balance as well. PPIs alter the level of acidity in our digestive tract. Stomach acid is our natural barrier against food-borne pathogens. PPIs weaken this sterilizing effect, leaving us more vulnerable to bacteria in food, which can infect the intestines. Also, less stomach acid means that some food might not be broken down sufficiently. What is not digested by our body can provide nourishment to bad bacteria.
All those effects can lead to bad bacteria colonizing the small intestines, a disease known as SIBO (small intestinal bacterial overgrowth). The consequences of poor intestinal bacteria balance include symptoms such as diarrhea, flatulence and constipation. While it is possible to heal SIBO, it is difficult and can take much time. When you already suffer from reflux, you do not want to add additional stress to your digestive system.
Acid Reflux Drugs Lose Their Efficacy Over Time
Even if you take PPIs, damage to the esophagus will continue to occur. The progression of the disease is only slowed down.
Sooner or later, the heartburn will come back, despite taking medication. Only this time, treating it is much more difficult, as the function of the esophagus will have deteriorated because of the chronic reflux. It’s still possible to treat heartburn at this stage, but the chances of success are lower and it takes much more time and effort. Therefore, it is vital to treat reflux early, instead of just popping a PPI that deals with the pain.
Reduced Absorption of Vitamins and Minerals
Gastric acid is essential for your body to absorb nutrients. When taking PPIs, the absorption of those nutrients becomes reduced.
Research has shown that iron, magnesium, zinc, and calcium are some minerals that are affected.[10],[11]
The most severely affected nutrient is vitamin B12, and this poses a massive problem our health.
Even a tiny 20mg dose of the PPI Omeprazole reduces the body’s absorption of vitamin B12 by 72%. A more common dose of omeprazole, 40mg, reduces absorption by as much as 88%.
This is a huge problem!
Vitamin B12 is vital for our nervous system. A B12 deficiency leads to, among other things, gradual damage to our nerves and irreversible neurological symptoms.
Luckily, our body has long-lasting stores of vitamin B12 because it is so essential for our health. A short-term course of treatment, lasting a few weeks to a few months, rarely causes deficiencies in otherwise healthy people.
PPIs Are Abused as Long-Term Treatment
However, many patients are prescribed proton-pump inhibitors for years or even decades. They are addictive. Without making changes to diet and lifestyle, it is very unlikely that a patient will manage to get off them.
PPIs should only be used as a short-term treatment - a quick relief, like a band-aid, to give your body time to heal while you change your eating habits at the same time. But this is rarely how acid reflux medication is used. PPIs are mistaken for medication that you can take forever.
12. The Surgery Option: Relief for the Most Severe Cases
Surgery is rarely required for heartburn.
However, for extreme reflux cases the most established and effective procedure is the Nissen Fundoplication. It has been the go-to surgery for decades. For cases of medium severity, the newer Stretta procedure can be helpful.
There are some other new procedures. However most are just filling the pockets of their inventors, without offering advantages for patients.
That being said, do not despair. As mentioned above, surgery only makes sense for a very small percentage of heartburn cases. A surgeon once told me that surgery is only the best option for about 1% of chronic acid reflux cases.
13. Diet: A Crucial Part of the Solution
Diet is by far the most important aspect in the treatment of heartburn; in fact, some reflux cases are related directly to diet alone.
Even if your heartburn has other underlying causes, a change in your diet will still help to control the symptoms. One way of accomplishing this is by avoiding known reflux triggers.
There is a lot of advice out there on diets for heartburn. And much of that advice is conflicted. Often, it’s simply general wisdom that is not backed up by studies. You don’t want to restrict yourself unnecessarily, but instead make a few effective changes in how and what you eat.
That is why I wrote my book How to Cure Heartburn without Pills, where I take an in-depth look at the methods that really work for healing heartburn. The book is primarily focused on diet and eliminating reflux triggers, but also contains information about other methods, like medical procedures. It’s a complete resource to help you get rid of your heartburn, naturally and effectively.
References
[1] Farré R, Sifrim D. Regulation of basal tone, relaxation and contraction of the lower oesophageal sphincter. Relevance to drug discovery for oesophageal disorders. Br J Pharmacol. 2007;153(5):858–869.
[2] Esophageal Cancer. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/esophageal/esophageal-cancer/precancerous-conditions/?region=on. Abgerufen am 24.04.2019.
[3] Mearin F, Malagelada JR. OESO foundation. How can the frequent absence of symptoms in severe reflux esophagitis be explained? https://www.hon.ch/OESO/books/Vol_5_Eso_Junction/Articles/art190.html. Mai 1998. Abgerufen am 24.04.2019.
[4] Woodland P, Shen Ooi JL, Grassi F, Nikaki K, Lee C, Evans JA, Koukias N, Triantos C, McDonald SA, Peiris M, Aktar R, Blackshaw LA, Sifrim D. Superficial Esophageal Mucosal Afferent Nerves May Contribute to Reflux Hypersensitivity in Nonerosive Reflux Disease. Gastroenterology. 2017;153(5):1230-1239.
[5] Banerjee B, Medda BK, Lazarova Z, Bansal N, Shaker R, Sengupta JN. Effect of reflux-induced inflammation on transient receptor potential vanilloid one (TRPV1) expression in primary sensory neurons innervating the oesophagus of rats. Neurogastroenterol Motil. 2007 Aug;19(8):681-91.
[6] Holzer P. Acid-sensitive ion channels and receptors. Handb Exp Pharmacol. 2009;(194):283–332.
[7] Bhat YM, Bielefeldt K. Capsaicin receptor (TRPV1) and non-erosive reflux disease. Eur J Gastroenterol Hepatol. 2006;18(3):263-70.
[8] Chrysos E, Prokopakis G, Athanasakis E, Pechlivanides G, Tsiaoussis J, Mantides A, Xynos E. Factors affecting esophageal motility in gastroesophageal reflux disease. Arch Surg. 2003 Mar;138(3):241-6.
[9] Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therap Adv Gastroenterol. 2012;5(4):219–232.
[10] Ito T, Jensen RT. Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium. Curr Gastroenterol Rep. 2010;12(6):448–457.
[11] Heidelbaugh JJ. Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications. Ther Adv Drug Saf. 2013;4(3):125–133.

