Battling the troublesome symptoms of silent reflux? Discover effective dietary strategies for relief.
In this article, we’ll share practical tips and strategies that may help you find both quick relief and long-term solutions for managing LPR.
LPR Nutrition: Key Points
- Food selection: Aim to cook with low-fat, low-acid, and easily digestible ingredients.
- Trigger foods to avoid: It’s essential to steer clear of certain foods known to potentially trigger reflux, such as garlic, chocolate, and coffee.
- Initial dietary change: Consider starting with a strict diet for the first two weeks, which may help quickly alleviate symptoms.
- Maintenance diet: After the initial phase, gradually reintroduce various foods to help identify your personal triggers.
- Eating habits: Pay attention not only to “what” you eat but also “when” and “how much.” Smaller, more frequent meals and avoiding late dinners before bedtime could make a significant difference.
- Long-term goal: The ultimate aim is to achieve lasting relief from reflux symptoms and improve your overall quality of life.
Three Fundamental Principles of the Silent Reflux Diet
When searching online, you’ll often come across various tips, tables, and food lists recommended for managing silent reflux. To better understand these recommendations, it’s helpful to grasp the basic principles behind the advice.
1) Smaller portion sizes:
- Why it matters: Large meals may increase stomach pressure and potentially overwhelm the lower esophageal sphincter (LES), leading to reflux.
- What to do: Try eating five smaller meals spread throughout the day instead of three large ones. This approach may help keep stomach pressure low and reduce the likelihood of silent reflux.
2) Avoiding potential reflux triggers:
- Why it matters: Some foods, such as fatty meals, chocolate, coffee, and alcohol, may relax the LES and increase the risk of reflux.
- What to do: Consider limiting or avoiding foods that could relax the LES.
3) Minimizing mucous membrane irritants:
- Why it matters: Certain foods may further irritate the mucous membranes already affected by stomach acid and digestive enzymes.
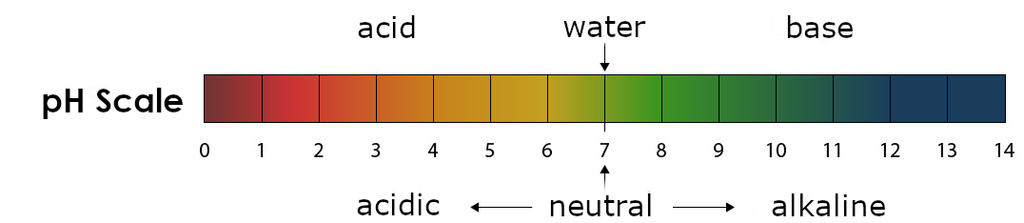
- What to do: Consider reducing foods that could irritate the mucous membranes, such as highly spiced dishes, high-proof alcohol, and acidic foods like citrus fruits and soft drinks.
Throughout the rest of the article, we’ll explore concrete measures you can take to incorporate these dietary principles into your daily life.
Foods That May Trigger Silent Reflux
When adjusting your diet to manage laryngopharyngeal reflux, consider limiting or avoiding these foods and drinks:
Remember, a small piece of chocolate or a cup of coffee may cause fewer symptoms than larger amounts. The same applies to the amount of spice in your recipes. A small pinch of pepper in the soup may have less effect on reflux than a whole teaspoon.
Examples of Meals That Could Frequently Trigger Silent Reflux
Some dishes may contain many potential reflux triggers. Here are a few examples of meals that might be less suitable for those with LPR:
Cooking at home may be generally better for managing reflux, as it’s easier to avoid potential triggers.
Of course, the recipe also matters. For example, you could prepare a Bolognese sauce that may be less likely to trigger reflux by omitting garlic, using fewer tomatoes, and using lean ground beef.
Recommended Foods
Here is a list of ingredients that may be recommended when cooking for silent reflux:
Fat-free protein sources, such as chicken and tofu, may be highly recommended for silent reflux.
Macronutrients: Composition of a Silent Reflux Diet
Macronutrients, which include fats, proteins, and carbohydrates, may have a direct impact on your silent reflux depending on their proportion in your diet.
Fats: Fatty foods may worsen LPR, as they could promote relaxation of the LES and slow gastric emptying. Therefore, it may be recommended to reduce the consumption of high-fat foods. However, in recent years, there have been questions in the scientific community about whether fat itself is the core problem, or rather that most fatty foods also come in large quantities and in combination with other potential reflux triggers. For example, many fatty dishes are fried, too large, or meat-based.
Proteins: Proteins may act oppositely to fats by potentially strengthening the tension of the LES. Lean protein like poultry, fish, and legumes may be beneficial for a reflux diet.
Carbohydrates: In general, carbohydrates may have no direct influence on silent reflux. They are often emphasized in recipes for the first phase of the reflux diet to minimize the proportion of high-fat foods as much as possible. Complex carbohydrates like whole grain products may be preferable as they could promote overall digestive system health and thus potentially positively influence LPR.
Special note on carbohydrates: In a small group of individuals, carbohydrates may trigger reflux symptoms, especially if small intestinal bacterial overgrowth is present. In this case, carbohydrate consumption could lead to excessive gas formation, putting pressure on the stomach and potentially exacerbating silent reflux.
Daily Meal Plan for Silent Reflux
A balanced meal plan with three main meals and two small snacks may be ideal for managing silent reflux. It’s important to keep dinner light so it can be digested by bedtime. Here’s an example nutrition plan that offers both meat and vegan cooking options:
Breakfast: A bowl of oatmeal with bananas, blueberries, and some nuts.
Morning snack: A glass of milk or a small handful of almonds.
Lunch: Chicken or tofu, served with quinoa and steamed vegetables.
Afternoon snack: A small roll or a slice of bread with low-fat cheese or a vegan topping.
Dinner: Baked salmon or a lentil dish, accompanied by some sweet potato mash and a small mixed salad.
These meals are designed to potentially minimize aggravating the symptoms of silent reflux while providing a balanced and nutritious diet.
Identifying Your Personal Triggers for LPR
Over time, it may be possible to gradually reintroduce foods that don’t seem to cause symptoms back into your diet.
Keeping a food and symptom diary could be extremely helpful. It may allow you to better understand the connections between your food intake and reflux symptoms and to recognize which specific factors might influence your symptoms.
Diet Progression
Dr. Jamie Koufman, a leading expert in the treatment of silent reflux, recommends a two-phase diet approach.
1) Initial Diet: Rapid Symptom Relief
- Duration: 2 weeks
- Approach: Consistently reduce known potential triggers of silent reflux, as described in the nutritional tips.
- Goal: Rapid relief of reflux symptoms by eliminating the main suspected triggers.
2) Maintenance Phase: Transition to New Eating Routine
- Duration: Permanent or until symptoms are completely resolved.
- Approach: Gradually reintroduce various foods to observe what is well tolerated and what may worsen silent reflux.
- Goal: Complete resolution of symptoms with minimal dietary restrictions. This phase offers more flexibility and allows for individual adjustments. Experiments with potential reflux triggers can be undertaken to expand the variety of tolerable foods. In the long term, the diet should be as normal as possible, with only the most necessary restrictions.
Conclusion on Diet for Silent Reflux
An adjusted diet may play a crucial role in the therapy and control of LPR.
The dietary change often begins with a stricter initial diet to quickly relieve symptoms, followed by a long-term maintenance phase in which foods are gradually reintroduced and tested for tolerability. It may be equally important to pay attention to portion sizes and spread meals throughout the day to avoid potentially overloading the LES.
For detailed tips and help on effectively relieving the symptoms of silent reflux, I recommend my online course, the “LPR Solution Blueprint“.









