Are you thinking about undergoing a fundoplication?
For example, a Nissen fundoplication?
If you have extreme acid reflux, that might be a good idea. Especially if nothing else has worked.
However, if you get an inexperienced surgeon, you might end up making it worse! Many doctors recommend surgery too early, even without having all the facts on your case themselves.
Surgeons get paid for cutting, not for talking!
Acid reflux is caused by many different factors. Fundoplication does not address all of them.
It can be difficult to tell whether your surgeon has your best interest in mind. To identify good surgeons, you will need advanced knowledge about acid reflux surgeries. That’s what I’m going to help you with in this article.
But first, let’s quickly cover the basics.
What’s Being Done During a Fundoplication?
Between your stomach and esophagus is a valve that keeps food in the stomach. This valve is called the lower esophageal sphincter, or LES.
If you have acid reflux, this valve is leaking. The purpose of the fundoplication is to fix the leak.
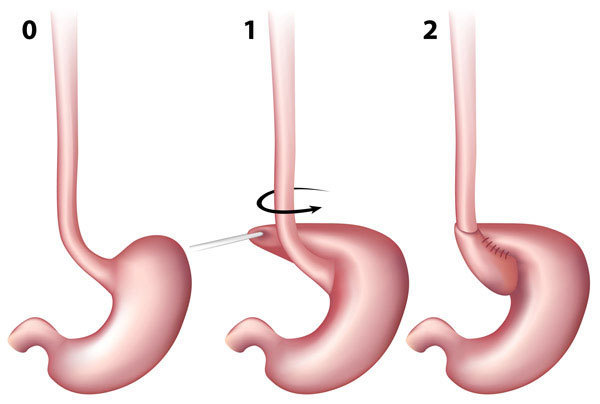
During the fundoplication, the upper part of the stomach is wrapped around the esophagus. This tightens up the valve. If it is done right, reflux is stopped or at least massively reduced.
There are different types of fundoplication.
The most common by far is the Nissen fundoplication. It is a tight 360-degree wrap. The stomach is wrapped all the way around the esophagus. The image above shows a Nissen wrap.
A Toupet fundoplication uses a weaker 270-degree wrap.
Why are there different types of fundoplication? We will talk about that later in the article.
Upsides of the Nissen Fundoplication: Decades of Experience
Developed in the 1950s by the German surgeon Dr. Rudolph Nissen, the Nissen fundoplication is by far the oldest reflux surgery in existence.
In the past, the entire chest had to be cut open to perform a fundoplication. Today, it is done as a laparoscopic fundoplication, which means it is less invasive. The surgeon makes a few small cuts and inserts a camera and his instruments, thereby avoiding the risks associated with open-chest surgery. The laparoscopic Nissen fundoplication has the distinct advantage of fewer complications and quicker recovery.
Because the Fundoplication is both the oldest and by far most common reflux surgery, it offers two important advantages:
1) Strong Scientific Foundation
Many studies have proven the long-term success of the fundoplication surgery. You are not being used as a guinea pig.
2) Surgeons with Profound Experience
The more a doctor performs a specific surgery, the better he gets at it.
Experienced surgeons have higher success rates for stopping reflux. They can also prevent complications.
You can find many surgeons and hospitals that have extensive experience in Nissen fundoplication surgery.
However, the same cannot be said for newer anti-reflux procedures like the LINX or the TIF. They simply have not been on the market long enough, which means there aren’t as many surgeons with the same level of experience as for the Nissen procedure.
Aside from the fundoplication, all acid reflux surgeries are experimental. One exception is the Stretta procedure, which already has 10-year data. This procedure works with electrical stimulation, which causes the sphincter muscle to grow over time. However, the Stretta can only cure light to medium reflux. For severe cases it will not be enough.[1] It also takes up to a year to see the full effect of the Stretta procedure, while the fundoplication works immediately.
Two in One: Repairing Hiatal Hernias During a Fundoplication
Many patients with reflux also have a hiatal hernia, a condition causing the stomach to slip above the diaphragm.
A hiatal hernia can increase reflux.
If you have a hiatal hernia, it can usually be repaired during the fundoplication, as it is very easy to do both at once. The surgeon is already operating on the same area anyway.
Most people’s hernias are small. I’m just pointing that out because I often get emails regarding this. Readers are confused about whether anti-reflux diets will help them heal despite a hiatal hernia. But a hiatal hernia is just one contributor to reflux. In nearly all cases, other factors are the main cause of reflux.
Does the Nissen Fundoplication Help With Respiratory Reflux?
Fundoplication is not only helpful for heartburn, but also for patients suffering from airway reflux, better known as silent reflux or LPR. Some typical symptoms include hoarseness, coughing, and asthma.
The Nissen fundoplication is the only surgery with a reasonable number of studies demonstrating it to be successful for the treatment of respiratory reflux.[2]
Complications Are More Common Than Your Surgeon Might Tell You
Wrapping the upper part of the stomach around the esophagus is highly unnatural. And whenever something is very unnatural, side effects are likely.
Bloating
A bloated belly is a very common side effect of the fundoplication.
During digestion, our body produces gas, mostly in our intestines, and, to a lesser degree, in our stomach. What’s more, when we eat we will also swallow some air involuntarily. In normal circumstances that's not a big deal. We burp or pass wind and that’s it.
However, the fundoplication creates a valve so tight that burping can become impossible.
Gas becomes trapped inside your belly. The result: bloating.
Bloating affects around 10% of all Nissen fundoplication patients.[3]
In mild cases it is an aesthetic issue at most. The belly will look bigger. However, in more severe cases, trapped air can lead to a lot of discomfort.Difficulty Swallowing
In some patients, the surgery leads to difficulty swallowing. That's not surprising: the lower esophageal sphincter is now tighter. The body is not used to pushing food through such a tight valve. Plus, the area around the sphincter is usually swollen right after surgery.
Swallowing difficulties are expected after a fundoplication. They usually get better by themselves within a few weeks or months. If they don’t improve, it’s likely that something is wrong with your wrap, for example it may be too tight. Seeing the surgeon or a gastroenterologist will help you find out what went wrong and find a solution.
Damaged Vagus Nerve
The vagus nerve controls our digestive system, including the valve between the stomach and esophagus. When the surgeon is carrying out the fundoplication, he must be very careful not to injure the nerve.
Officially, damage to the vagus nerve during surgery is rare; it’s certainly something that has received very little attention in research.
However, when you do a little digging, the picture looks very different.Vagus nerve injuries are a surprisingly common result of anti-reflux surgeries.
Various studies have put the risk of vagus nerve injury caused by a fundoplication between 10% and 42%.[4], [5], [6], [7]
This is a massive range. It shows how little certainty there is on how the vagus is affected by a fundoplication. One review stated that “[accidental vagus nerve injury] is much higher than previously assumed” and that it is a “generally neglected complication.”
What does that mean for you? Should you avoid this surgery because of the risks?
Well, let’s look at the bright side first. Even if the vagus nerve gets damaged, your reflux will most likely still be better after surgery.
However, in the long term, the risk of developing reflux again is higher with a damaged vagus nerve.[8]
Plus, a damaged vagus nerve can wreak havoc to our digestive system. It can lead to symptoms like diarrhea, dumping syndrome or nausea. A damaged vagus can increase the risk of most kinds of digestive disease.[9], [10]
Not All Fundoplications Last Forever
Fundoplications tend to become less effective over time. The reflux can come back.
There are two reasons for this:
1) Slipping or Damaged Fundoplication
The wrap must stay around the lower esophageal sphincter for the fundoplication to work.
Sometimes the wrap slips, sutures rip, or it completely un-wraps. It can happen when the surgeon did a bad job. Sometimes it’s just bad luck.
Heavy lifting is a typical cause for damaged fundoplication. Lifting heavy weights causes the abdominal muscles to put massive pressure on the stomach, including on the fundoplication wrap, which is formed by the upper part of the stomach. That is why bodybuilders and construction workers have a higher risk of damaged fundoplications.
2) Loosening Up of the Wrap
The wrap around the stomach becomes dilated each time we swallow something.
Overeating makes this worse. It puts considerable stress on the valve.
Over time, this regular stress can cause the fundoplication to become loose. That is why a fundoplication is not a free pass to indulge in whatever food you want! You still need to take care of how much you eat.
Different Types of Fundoplication
Fundoplications vary in the way the stomach is wrapped around the lower esophageal sphincter.
Most patients either get a Nissen or a Toupet fundoplication. Nissen works better against reflux, but Toupet produces fewer side-effects.
Nissen Fundoplication (Full 360° Wrap)
The Nissen fundoplication is the by far most common variant. The upper part of the stomach is wrapped all the way around the valve. The result is a 360-degree wrap.
Nissen is the most effective fundoplication against reflux because it creates a tighter valve.Results of the Nissen Fundoplication for Heartburn
After the surgery, heartburn is removed in 98% of all patients.
However, heartburn can come back. After 10 years, about a quarter of patients experience heartburn again, usually because the fundoplication has become loose. A second surgery might be able to fix the reoccurring heartburn.
The disadvantage of the Nissen is that side-effects are more pronounced than with a partial Toupet fundoplication.
Nissen for Airway Reflux
This part is for people with airway reflux. It shows up with symptoms like hoarseness, chronic coughing and asthma.
Studies show that the Nissen surgery for airway reflux delivers varying results. The main reason for that is disagreement on how to diagnose airway reflux. Some use complex testing. Others simply include people that report symptoms of airway reflux. Some studies include people who do not actually have airway reflux. These factors make certain studies inaccurate.
According to one study published by the American Surgeon journal, the Nissen fundoplication improved airway reflux symptoms in 75% of patients. Think about what this means. Not that they were healed. Just that 3 in 4 patients experienced some kind of improvement. Some might be cured, sure. But we can’t tell from that study.
Another study looked at how much people with airway reflux got better. Their symptom score improved from an average of 31.7 (extreme symptoms) to 10 (mild symptoms).
To sum it up: the Nissen fundoplication works well for a good percentage of airway reflux patients. But the success rate is far lower than for heartburn. It is a good option for extreme cases, but most should look at other options. Take a look at my detailed article on the treatment of airway reflux.
Toupet Fundoplication (partial 270° wrap)
You could call the Toupet fundoplication Nissen’s little brother.
Toupet form a partial 270-degrees wrap. This means the wrap goes only three quarters of the way around the esophagus, instead of all the way like the Nissen does.
The Toupet wrap is not as tight, which means reflux is not stopped as effectively as with the Nissen fundoplication.
The reason why a Toupet is still sometimes carried out is that a looser wrap also means fewer side-effects. Some people simply can’t tolerate a tight wrap for different physiological reasons. Those reasons might show up during the pre-surgery tests. Sometimes a Nissen is also changed into a Toupet during a second surgery. It can relieve certain common side-effects like bloating or swallowing issues.
Surgery Should Be the Last Resort Only
The fundoplication can certainly help the most severe cases of reflux.
However, this surgery is sold as having a low complication rate, and that is a lie. The fundoplication comes with some major risks. It can lead to permanent side-effects. It does not always work. And even if it does, it can sometimes become loose and a second surgery is required.
Surgery is often done too quickly, before having explored all other options. For example, changes in diet and lifestyle can be extremely effective. For patients with airway reflux, my online course covers all you need to know to get better.
I only recommend going for an anti-reflux surgery if all other measures have failed to provide you with relief. Which is rare.
References
[1] Triadafilopoulos G. Stretta: a valuable endoscopic treatment modality for gastroesophageal reflux disease. World J Gastroenterol. 2014;20(24):7730–7738.
[2] Mazzini Gda S, Gurski RR. Impact of laparoscopic fundoplication for the treatment of laryngopharyngeal reflux: review of the literature. Int J Otolaryngol. 2011;2012:291472.
[3] Carlson MA, Frantzides CT. Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg. 2001;193(4):428-39.
[4] Lindeboom MY, Ringers J, van Rijn PJ, Neijenhuis P, Stokkel MP, Masclee AA. Gastric emptying and vagus nerve function after laparoscopic partial fundoplication. Ann Surg. 2004;240(5):785–790.
[5] van Rijn S, Roebroek YG, Conchillo JM, Bouvy ND, Masclee AA. Effect of Vagus Nerve Injury on the Outcome of Antireflux Surgery: An Extensive Literature Review. Dig Surg. 2016;33(3):230-9.
[6] van Rijn S, Rinsma NF, van Herwaarden-Lindeboom MY, Ringers J, Gooszen HG, van Rijn PJ, Veenendaal RA, Conchillo JM, Bouvy ND, Masclee AA. Effect of Vagus Nerve Integrity on Short and Long-Term Efficacy of Antireflux Surgery. Am J Gastroenterol. 2016 Apr;111(4):508-15.
[7] DeVault KR, Swain JM, Wentling GK, Floch NR, Achem SR, Hinder RA. Evaluation of vagus nerve function before and after antireflux surgery. J Gastrointest Surg. 2004 Nov;8(7):883-8.
[8] van Rijn S, Rinsma NF, van Herwaarden-Lindeboom MY, Ringers J, Gooszen HG, van Rijn PJ, Veenendaal RA, Conchillo JM, Bouvy ND, Masclee AA. Effect of Vagus Nerve Integrity on Short and Long-Term Efficacy of Antireflux Surgery. Am J Gastroenterol. 2016 Apr;111(4):508-15.
[9] van Rijn S, Roebroek YG, Conchillo JM, Bouvy ND, Masclee AA. Effect of Vagus Nerve Injury on the Outcome of Antireflux Surgery: An Extensive Literature Review. Dig Surg. 2016;33(3):230-9.
[10] Spaziani R, Bayati A, Redmond K, Bajaj H, Mazzadi S, Bienenstock J, Collins SM, Kamath MV. Vagal dysfunction in irritable bowel syndrome assessed by rectal distension and baroreceptor sensitivity. Neurogastroenterol Motil. 2008 Apr;20(4):336-42